Abstract
Introduction
The 2-year survival for AML patients relapsing after allogeneic hematopoietic cell transplantation (alloHCT) is <20%, independent of the choice of relapse-treatment. Relapse detection in its molecular state enables early interventions and possibly prevention of hematological recurrence of the disease. The role of measurable residual disease (MRD) monitoring for risk stratification has been described for pre and post-alloHCT MRD analyses. Yet, it remains unclear, if and by which lead-time NGS assessment can detect MRD before impending relapse. We hypothesize that the functional class of mutations determines the relapse kinetics in AML after alloHCT.
Methods
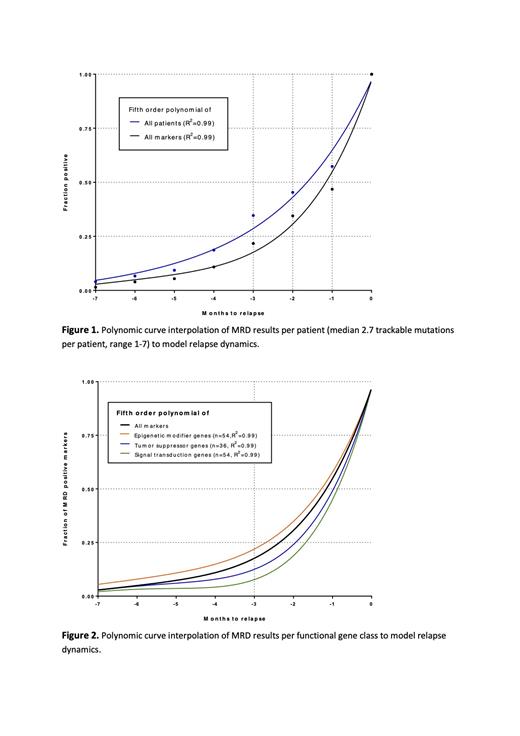
We identified mutations present at AML relapse after alloHCT by Illumina myeloid panel sequencing covering 48 AML associated genes. Peripheral whole blood samples were retrospectively collected before hematological relapse, with a minimum of one sample per patient at three months prior to relapse and if available, additional monthly samples. Amplicon-based NGS and bioinformatics error-correction were performed on those samples as described in Thol et al. 2018. Positive MRD was defined as MRD detectable above the limit of detection. In the last step, we performed polynomic curve interpolation to model relapse dynamics.
Results
MRD was assessed in 75 AML patients after alloHCT using 203 AML-related mutations present at the time of relapse, corresponding to a median of 2.7 trackable mutations per patient (range 1-7). In total, 305 MRD analyses were performed from peripheral blood (median 1.5 per mutation, range 1-5) prior to relapse. VAFs measured above the limit of detection (median LOD across all targets 0.0315) ranged from 0.0048-26% (median 1.3%).
In 45 of 75 patients (60%), we detected MRD in at least one sample and one marker before relapse. Of those, 23 patients (51%) were MRD positive in all markers before relapse and 22 patients (49%) were MRD positive in some, but not all markers before relapse. The majority of MRD-positive patients (30 of 45) were first detected three or fewer months before relapse, whereas 15 (33%) of 45 patients were MRD positive more than 3 months before relapse. The median time to relapse from the first MRD-positive sample to relapse was 2.9 months (range 0.6-10.2).
Among the 203 mutations found in relapse, 93 (46%) were detectable by MRD monitoring before relapse while the remaining 110 markers (54%) remained undetectable prior to relapse. Of note, 88 of those 110 markers (80%) were measured only once before relapse, indicating that frequent sampling increases the likelihood of MRD detection. Genes in which mutations were found mostly MRD-positive were TET2 (6 out of 6), ASXL2 (4 out of 5), SF3B1 (4 out of 5), and RUNX1 (7 out of 9). Mutations in WT1 (1 out of 13), NRAS (1 out of 8), FLT3-ITD (9 out of 29), and PTPN11 (1 out of 5) were among the most common MRD negative mutations before relapse.
To assess clonal relapse dynamics, pre-relapse samples were assigned to the monthly interval that best matched the sampling time. If MRD was measured positive at one time point, all the following monthly intervals were considered MRD-positive, whether a sample was available for that interval or not. The fraction of positive samples from all samples per time point was plotted against time to relapse and the function was approximated by fifth-order polynomials. The percentage of patients being MRD positive increased markedly with shortened distance to relapse. Thus, 29% of patients were MRD positive at 3 months, 44% at 2 months and 66% 1 month prior to relapse. Summarized by functional gene classes, mutations in tumor suppressor genes and especially signaling genes showed a higher slope and thus a shorter lead-time to relapse than mutations in epigenetic modifier genes (Figure 2).
Conclusion
In summary, hematologic relapse can be detected in peripheral blood in 29, 44, and 66% of patients at 3, 2, and 1 months before relapse by NGS-MRD analysis, respectively. Mutations in epigenetic modifier genes show a higher fraction of MRD positivity before relapse than other mutations. In contrast, mutations in signaling genes show a shorter lead-time to relapse.
Ganser: Celgene: Honoraria; Novartis: Honoraria; Jazz Pharmaceuticals: Honoraria. Thol: Abbvie: Honoraria; Astellas: Honoraria; Novartis: Honoraria; Pfizer: Honoraria; Jazz: Honoraria; BMS/Celgene: Honoraria, Research Funding. Heuser: BergenBio: Research Funding; Bayer Pharma AG: Research Funding; AbbVie: Membership on an entity's Board of Directors or advisory committees, Research Funding; BMS/Celgene: Membership on an entity's Board of Directors or advisory committees, Research Funding; Janssen: Honoraria; Novartis: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees, Research Funding; Pfizer: Membership on an entity's Board of Directors or advisory committees, Research Funding; Daiichi Sankyo: Membership on an entity's Board of Directors or advisory committees, Research Funding; Jazz: Honoraria, Membership on an entity's Board of Directors or advisory committees, Research Funding; Astellas: Research Funding; Tolremo: Membership on an entity's Board of Directors or advisory committees; Karyopharm: Research Funding; Roche: Membership on an entity's Board of Directors or advisory committees, Research Funding.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal